Caring for care providers
Our healthcare depends on the well-being of the people caring for us. However, health workers worldwide are in the midst of a crisis. It’s part labor crisis, part mental health crisis, part education crisis, part gender equality crisis, and part financial crisis. [1, 2, 3] The result is a global shortage of health workers. [4] There's not "the right number of people with the right skills in the right place at the right time to provide the right services to the right people." [5] This will become increasingly problematic under the pressures of population aging.
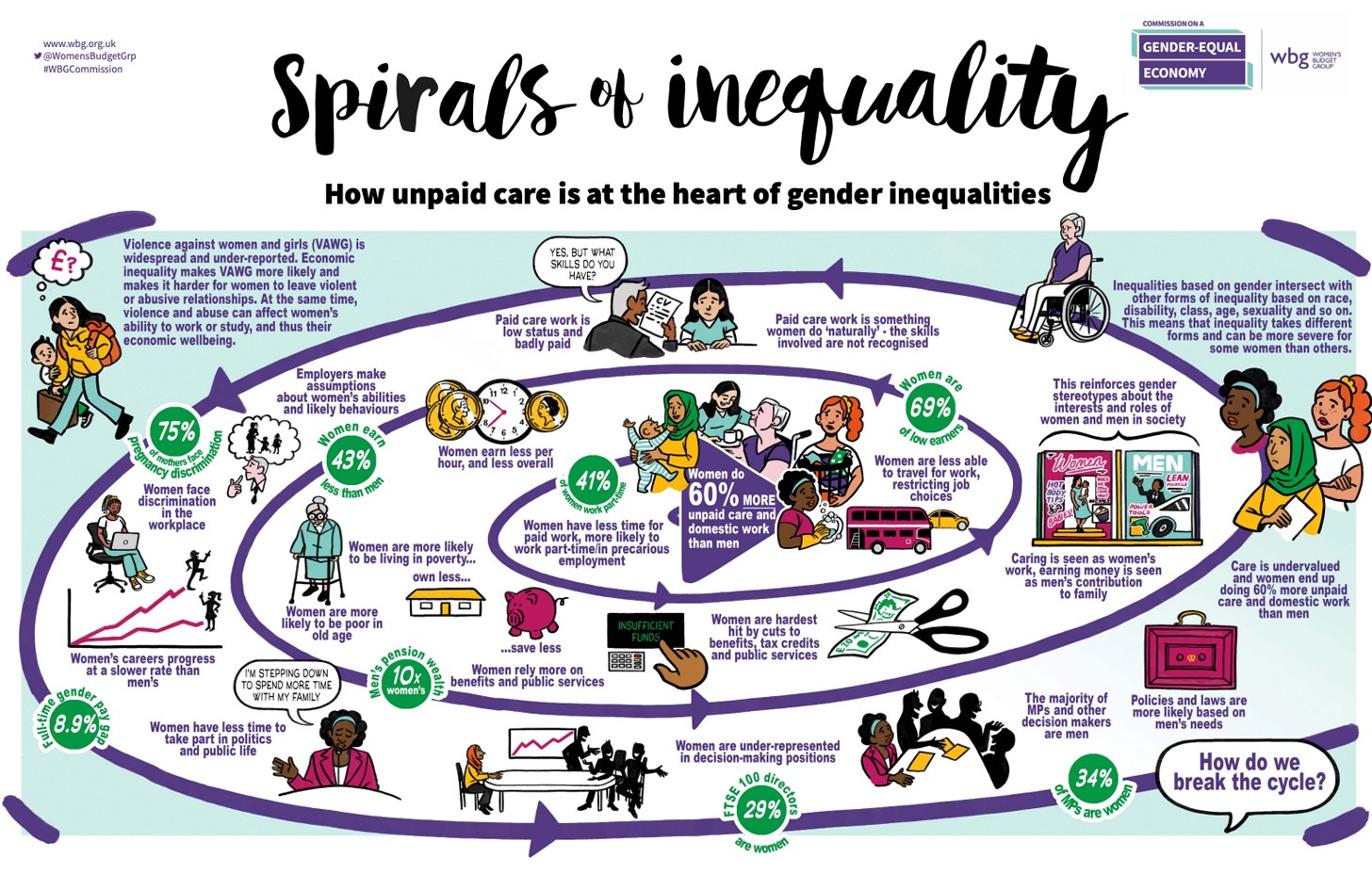
Many healthcare systems are currently upheld by unpaid and underpaid care workers. This work is at the heart of gender inequalities. [7]
Many healthcare systems are currently upheld by unpaid and underpaid care workers. This work is at the heart of gender inequalities. [7]
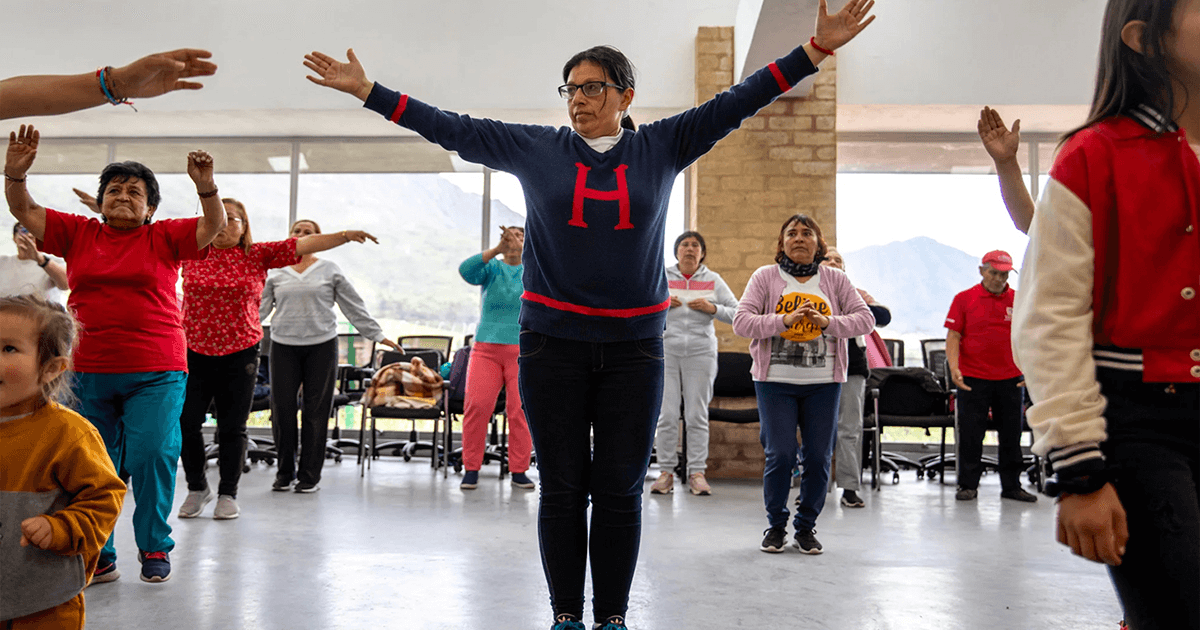
In Bogotá, 3.6 million women carry out unpaid care work. More than a million do so full-time. That's 30% of the population whose every day is "dictated by their responsibility to care for loved ones." This impacts every aspect of their well-being – physical, social, and economic. [8]
To address this inequality, the government "decided to bring the city and its services to caregivers and integrate these services into one [centralized] space," affectionately referred to as Manzanas del Cuidado or Care Blocks. [8] Each block provides a diversity of services – health, wellness, professional training, and education (for women and their families) – within a 15- to 20-minute walk for caregivers. [9]
"The motto of the care blocks is we take care of people that take care of others," notes [Home Care Coordinator] Ingrid Carbajal. "That's really important for the people that come here, because they begin to feel appreciated. They begin to feel recognized for the work that they're doing.'" [9]
To learn more about the key elements of the Care Blocks and the iterative approach to the policy design and implementation that underpins the initiative, check out the Urban Council’s interview featuring the Secretary of Women’s Affairs for Bogotá, Diana Rodríguez Franco. [10]
Signal 2: The U.S. Surgeon General’s Advisory
While burnout among U.S. health workers reached crisis levels before 2020, the Covid-19 pandemic amplified the effects. [11] Today, many health workers feel "exhausted, helpless, and heartbroken." [12] In response, U.S. Surgeon General Dr. Vivek Murthy has declared health worker burnout one of the most public health issues of our time. [13] And published an advisory in 2022 to begin building a thriving health workforce together. [12]
Why is this Advisory compelling?
It frames the crisis as a collective problem and opportunity.
It considers health workers' physical, social, economic, and environmental well-being. “When health workers look ahead, they should see a future where their dedication isn’t taken for granted, and where their health, safety, and well-being is as much a priority as the well-being of the people and communities in their care." [12]
It translates insights into actions that can unfold at various scales – from individual to organizational and cross.
It offers examples and resources.
And it calls attention to its limitations. "This Advisory contains steps that various stakeholders can take together to address health worker burnout. It calls for change in the systems, structures, and cultures that shape health care. Given the nature and complexity of the challenges outlined, this Advisory is not intended to be comprehensive in its recommendations." [12]
Hero image Source: Ben de la Cruz, NPR October 2023